Prevalence of eating disorder symptoms in people with insulin-dependent-diabetes: A systematic review and meta-analysis.
Published Date:
28th February 2024
Published By:
Pia E. Niemelä, Hanna A. Leppänen, Ari Voutilainen, Essi M. Möykkynen, Kirsi A. Virtanen, Anu A. Ruusunen, Reeta M. Rintamäki.
Approved By:
Yet to be
Decoded By:
Sian Callaghan
MSc Eating Disorders and Clinical Nutrition, BSc Psychology.
10 mins to read
- The T1D Takeaway
- Disordered eating behaviour in type one diabetes can lead to a greater risk of diabetic complications
- If you are experiencing symptoms of disordered eating, speak to your specialist diabetes team who can offer help and support.
Word Wizard
- A recent study showed that >60% of healthcare professionals working with people with diabetes expressed low confidence in identifying individuals living with type one diabetes who also had eating disorders.
- 78% of these healthcare professionals had no screening tool to identify disordered eating in the type one diabetic population
- Eating disorder symptoms were more common in women than men in this analysis. This may be due to a failure to notice eating disorder symptoms in men. However, this difference between biological sex is largely misunderstood.

Summary Snap
Shots
This research aims to examine the prevalence of eating disorder symptoms in people with insulin-dependent diabetes who were aged 16 or over
Prime Insight
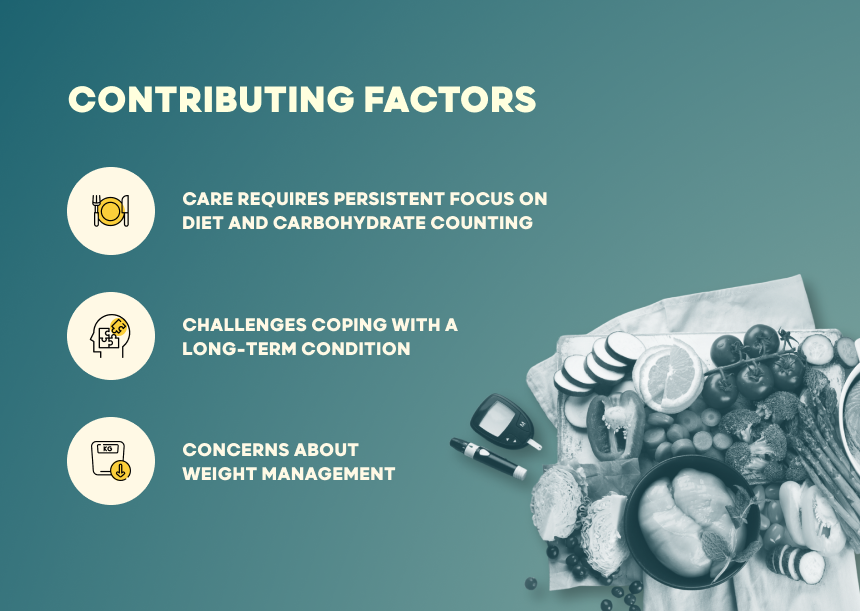
Eating disorders are more prevalent in people with diabetes than in the general population. People with insulin-dependent diabetes are at greater risk of developing eating disorders due to several factors. These include:
- Focus on diet and carbohydrate counting
- Difficulties coping with a long-term condition
- Concerns over shape and weight
78% of these healthcare professionals had no screening tool to identify disordered eating in the type one diabetic population
Individuals with type one diabetes, or those with type two diabetes who use insulin, often engage in the condition-specific behavior of insulin omission. This refers to intentionally skipping insulin doses to lose weight. This can be very damaging to health as it leads to high blood sugar leading to life-threatening emergencies, including diabetic ketoacidosis (DKA). Insulin omission leads to more diabetic complications than other weight control behaviours. However, recent studies suggest that, for those who omit insulin, the desire to lose weight is more important than the risk of complications due to high blood sugar. As a result of this, healthcare professionals may feel ill-equipped to treat both comorbidities simultaneously.
- The authors analyzed the current literature on eating disorder symptoms in individuals with insulin-dependent diabetes
- 24-27% of individuals examined in the study experienced eating disorder symptoms. These symptoms were more common in men than women.
- 21% of individuals examined restricted their insulin usage as a means of controlling their body weight
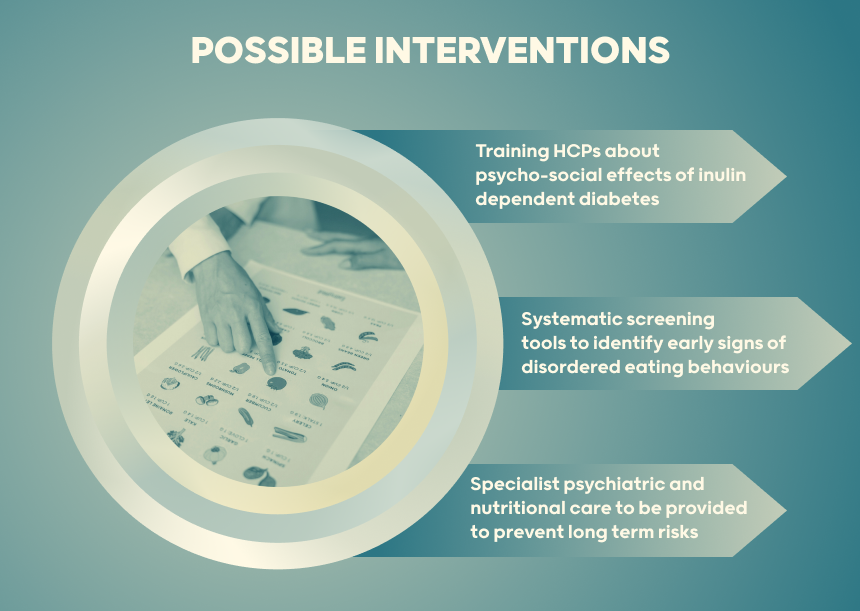
Early recognition and appropriate treatment are vital for treating disordered eating behaviour in those with insulin-dependent diabetes.
The future aim should be to identify patients with eating disorder symptoms by systematic screening, as co-occurring eating disorders and type one diabetes increase the risk of diabetic complications, hospital admission rates and risk of death when compared with patients with type one diabetes without an eating disorder.
When disordered eating behaviours are recognised by healthcare professionals, specialist psychiatric and nutritional care can be provided. However, more research and training is needed as healthcare professionals can often fail to sympathize with the psychosocial effects and emotional issues related to living with insulin-dependent diabetes.
- A Deeper Dive
- The Sources Voice
Eating disorder symptoms and insulin omission are common in patients with insulin-dependent diabetes regardless of age. Studies with a higher proportion of female participants report higher prevalence rates.
- Curiosities Clarified
Those with insulin-dependent diabetes can omit insulin as a means of weight control, which can lead to diabetic complications and even death
- Disordered eating behaviours may be more common in those with insulin dependent diabetes as the condition relies on a heavy focus on diet, and can be an emotionally challenging condition to live with
It is important that healthcare professionals receive enough training so that they feel confident and competent in identifying and addressing comorbid disordered eating behaviours and insulin-dependent diabetes. Adequate screening tools are needed to assist with this identification.
2 Comments
If you are looking for Bulk email sending software with allow unlimited smtp,subject,body messsage,attachments then Qualify Bulk Mailer is the Best Bulk email sender software.
Hello dcodeddiabetes.com admin, Your posts are always well-delivered and engaging.