Association between Continuous Glucose Monitoring metrics and clinical outcomes in adults with Type 1 Diabetes in a real-world setting.
Published Date:
April 30, 2024
Published By:
Robert Brett McQueen, Magaly Perez-Nieves, G Todd Alonso, Ludi Fan, Emily R Hankosky, Viral N Shah, Yuer Yan, Samuel L Ellis, Rattan Juneja.
Approved By:
Decoded By:
Asra H. Ahmed
MBA, PGCE in Assessment Learning disability, Diabesties Foundation.
10 mins to read
- The T1D Takeaway
- A CGM is just better for me! I can justify and advocate for my providers to give me access to a continuous glucose monitor. (Eversence, DexcomG6 or G7, Libre 2, libre3 and the Medronic Simplera monitors) are not just tech accerires, but essential for better type 1 diabetes management.
Word Wizard
- Researchers analyzed real-world data to check if the expert-recommended CGM targets work as well outside of controlled trials.
- The research examined real-world CGM and clinical data to evaluate these targets.
- When looking at data from real people living with type 1 diabetes, they found that for every 10% increase in the amount of time they kept their blood sugar within the target range, their HbA1c (a measure of long-term blood sugar control) dropped by 0.34%. This decrease was smaller than what was seen in controlled trials.
- The study found that how HbA1c, blood sugar fluctuations, and episodes of low blood sugar (hypoglycemia) relate to each other is complicated and not straightforward.
- These relationships might differ in actual clinical practice compared to controlled trials.
Summary Snap
Shots
When looking at data from real people living with type 1 diabetes, it was found that for every 10% increase in the time their blood sugar was in the target range, their HbA1c (a long-term blood sugar measure) dropped by 0.34%. This drop was smaller than in controlled trials.
Prime Insight
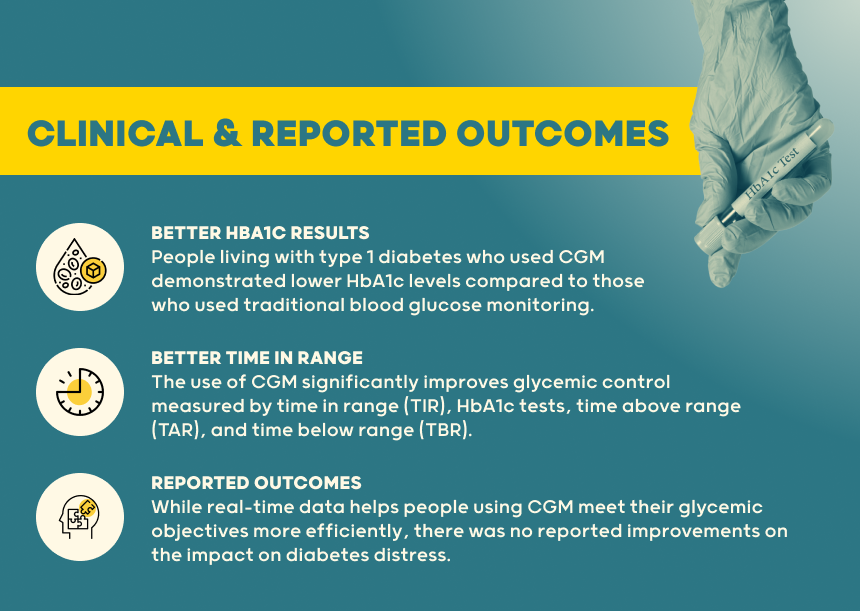
Glycemic Control Improvements: The use of CGM significantly improves glycemic control measured by time in range (TIR), HbA1c tests, time above range (TAR), and time below range (TBR). These improvements were associated with better overall glycemic management and reduced hypoglycemia incidence.
CGM use to measure blood glucose levels was found to improve clinical outcomes among people living with type 1 diabetes.
even though their effect on how individuals feel about wearing a device can vary. Using CGM in regular care is important for better diabetes management and fewer complications.
Clinical Outcomes: People living with type 1 diabetes who used CGM demonstrated lower HbA1c levels compared to those who used traditional blood glucose monitoring. Additionally, CGM usage was linked to reductions in glycemic variability, which is crucial for minimizing the risk of both acute and long-term diabetes complications.
Reported Outcomes: People living with type 1 diabetes reported significant improvements in Glycemic objectives. However, there was no reported improvements on the impact on diabetes distress, fear of hypoglycemia, and overall well-being.
Adherence and Effectiveness: Adherence to CGM usage plays a critical role in achieving these benefits. Higher adherence rates correlate with better glycemic control and more significant clinical improvements.
Real-World Applicability: The study emphasizes that CGM provides a more comprehensive picture of glucose trends and fluctuations compared to HbA1c alone. This real-time data allows for more responsive and personalized diabetes management, which is particularly beneficial in a real-world setting
- A Deeper Dive
- The Sources Voice
This study quantifies HbA1c improvements with increased TIR and hypoglycemia reductions with improved CV in clinical practice.
- Curiosities Clarified
The study found that improved CGM metrics, such as increased time in range were significantly associated with better glycemic control and fewer diabetes-related complications.
CGM use led to significant improvements in HbA1c levels and more stable blood glucose levels, demonstrating its effectiveness in managing type 1 diabetes.
The study highlighted the importance of integrating CGM into standard diabetes care, as consistent use of CGM devices was shown to help achieve optimal glycemic control and reduce the risk of complications.
The study explores the variability in outcomes, such as quality of life and diabetes-related stress, to see if there is a consistent improvement in these areas with CGM use. This aspect assesses the psychological and emotional impacts of continuous glucose monitoring among people living with type 1 diabetes.