An unwelcome inheritance: childhood obesity after diabetes in pregnancy
Published Date:
13 July 2023.
Published By:
Approved By:
To be
Decoded By:
Sian Callaghan, MSc Eating Disorders and Clinical Nutrition, BSc Psychology.
10 mins to read
- The T1D Takeaway
- For those living with type one diabetes who are pregnant or hoping to conceive, weight management and well-controlled blood sugar levels during pregnancy may be important to help optimize the health outcomes of their child
- Those hoping to conceive should speak to their healthcare team to address any potential risk factors, and to receive intervention where appropriate
Word Wizard
- This research aims to better understand the connection between diabetes in pregnancy, and subsequent childhood obesity
- Associations have previously been identified between diabetes in pregnancy and childhood obesity, body fat and thickness of skinfolds (a common method used to measure body fat). This effect has been observed regardless of the type of diabetes the mother has; what is important is the severity of high blood sugar (hyperglycaemia)
- There are several interventions that can be adopted pre-, during and post- pregnancy which may have a positive impact on infant birth weight and subsequent health outcomes.

Summary Snap
Shots
Diabetes in pregnancy is associated with an increased risk of high birth weight and childhood obesity; a phenomenon observed across European and Asian countries. Childhood obesity may have negative effects on health, including type two diabetes and poor heart health, and can be a determinant of levels of body fat into adulthood.
Prime Insight
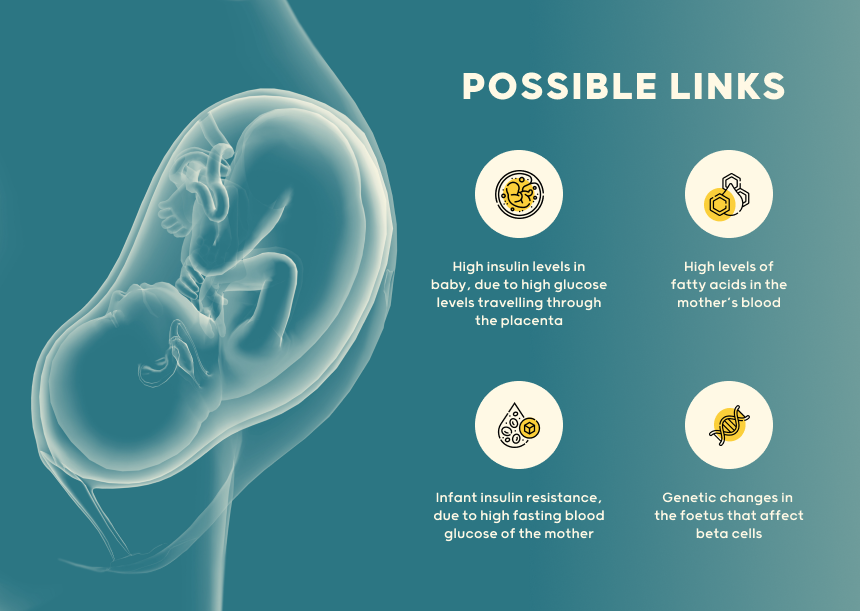
Why does diabetes in pregnancy lead to high infant birth weight?
It is currently not fully understood why diabetes in pregnancy may lead to increases in birth weight. Researchers have suggested the following reasons:
- Glucose is the main fuel source for both fetus and placenta. High glucose levels from the mother can travel across the placenta, giving the fetus abundant fuel. Fetuses will produce higher insulin levels in response to this glucose, which can lead to increased growth.
- Fatty acids in the mother’s blood are elevated in those with diabetes in pregnancy. These fatty acids are related to increased body fat in infants, regardless of blood sugar levels of the mother.
- Diabetes in pregnancy may lead to infant insulin resistance, as well as insulin resistance in later childhood, contributing to weight gain. These findings were not related to the weight of the mother or the child, but were related to fasting blood sugar levels.
- The EPICOM study found that diabetes during pregnancy led to genetic changes in the infant. These genetic changes may affect beta cell function (the cells which produce insulin in the pancreas).
Effective interventions targeting maternal high blood sugar, obesity and offspring health are needed to optimize the health of the child
Some outstanding questions remain in this area. Although we know that maternal blood sugar levels can impact birth weight of infants, we are yet to understand how this can have an impact on long term health outcomes for the child
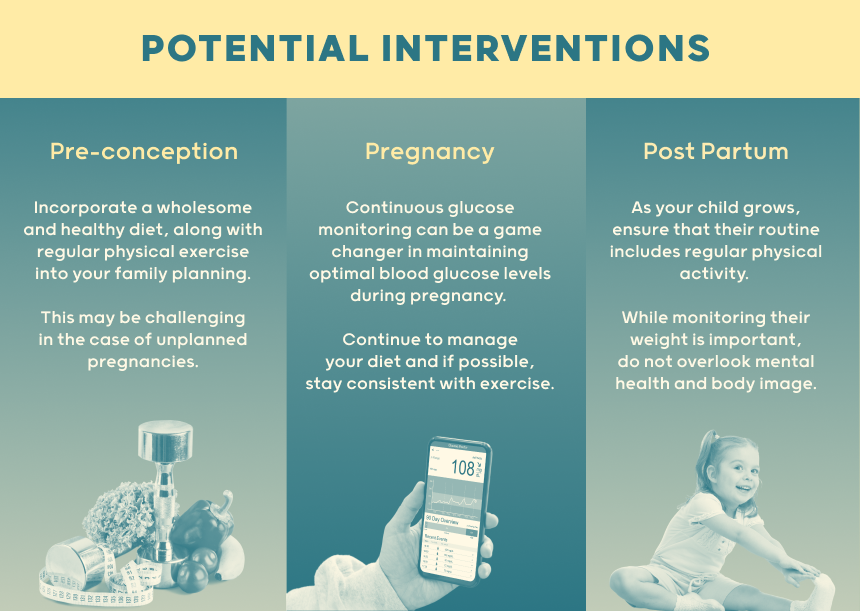
Potential interventions
Intervention will require a focus on maternal and infant health before, during and after pregnancy, to ensure the cycle of obesity from generation to generation does not continue.
Preconception (before pregnancy):
- Dietary and exercise interventions prior to pregnancy may help to optimize blood sugar levels. However, as many pregnancies are unplanned, providing support before conception can be challenging.
Pregnancy:
- Dietary management of gestational diabetes has been associated with lower birthweights, which may lead to benefits in future infant health outcomes. However, what constitutes the optimal diet for pregnant mothers is currently unclear.
- Continuous glucose monitoring may also help to reduce episodes of high blood sugar in type one diabetes.
- Excess weight gain during pregnancy may be related to childhood obesity. This excess weight gain should be monitored and interventions put in place accordingly.
Postpartum (after birth):
- Healthy diet, regular physical activity and environments which support a healthy lifestyle are important for the prevention of childhood obesity.
- New drugs, as well as surgeries, may help adolescents with obesity.
- The effects of childhood obesity on mental health and wellbeing need to be assessed and addressed.
- A Deeper Dive
- The Sources Voice
Exposure to maternal diabetes and/or obesity in utero is likely to influence offspring body composition, insulin sensitivity and beta cell function. While the mechanisms behind this are underexplored, the complex interplay between maternal and offspring insulin and lipid metabolism are likely to be involved. Effective intervention will require a new focus on maternal health before, during and after pregnancy to halt the intergenerational cycle of obesity.
- Curiosities Clarified
Research demonstrated that the link between diabetes in pregnancy and childhood obesity may be directly connected to the severity of hyperglycemia.
At present, it is not clear which intervention is most effective for reducing childhood obesity. However, a combination of prenatal, pregnancy and postnatal interventions should be adopted to optimize outcomes.
1 Comment
1msmyi